Preparation and characterization of CCDs
Using curcumin powder as the main raw material, combined with zinc ions provided by zinc acetate and nitrogen rich polyethyleneimine, a brownish yellow carbon dots powder was finally obtained through a classic one-step hydrothermal method (Fig. 1A). During the synthesis process, some properties of the raw materials were well transferred to the new products. At the same time, various elements and electron pairs undergo reaction pairing and binding, giving CCDs new and unique properties.
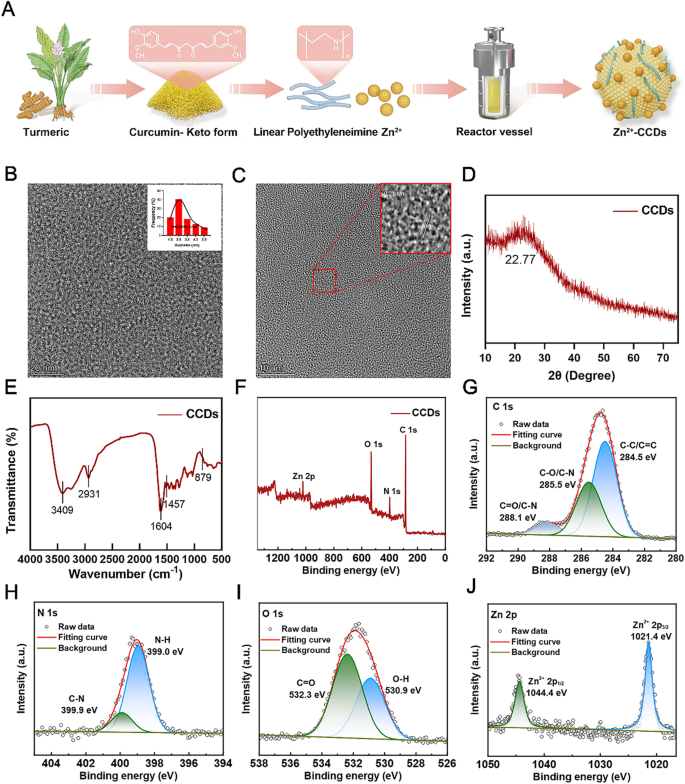
Characterization of CCDs. (A) Schematic illustration of the preparation process of CCDs; (B, C) TEM images and nanoparticle size analysis; (D) XRD pattern of CCDs; (E)FT-IR spectra of CCDs; (F) XPS full-scan spectrim of CCDs; XPS high-resolution scans of C1s (G), N1s (H), O1s (I) and Zn 2p (J) of CCDs.
Fig. 1B and C are TEM images of composite nanoparticles, showing that CCDs were spherical and had a uniform particle size distribution, with an average of 2.65 ± 0.3 nm. It can be seen that CCDs had detailed lattice fringes, and the lattice spacing corresponds to the (001) crystal plane of graphite at 0.21 nm, which was similar to the results reported in the literature [23]. The XRD pattern of the composite nanoparticles in Fig. 1D showed a clear peak of CCDs at 22.77 °, corresponding to the (002) crystal plane of graphite carbon, indicating that CCDs had a complete crystal structure and have been successfully prepared [24]. The surface of CCDs had a positive potential of 28.9 (Fig. S1), and the presence of multiple functional groups on the surface facilitates the response of CCDs to laser irradiation in various wavelength bands. Studies have shown that CCDs with positive potential can firmly bind to bacterial surfaces with negative potential, improving their bactericidal performance [25].
The FT-IR spectrum shown in Fig. 1E exhibited peaks at 3409, 3255, 2931, 1604, and 1457 cm− 1, corresponding to the stretching vibrations of – OH/- NH, C-H, C = C, and N-H groups, respectively. The peak at 879 cm− 1 could be considered a characteristic peak of ZnO, which is related to specific vibration modes in the ZnO crystal structure. Therefore, the significant water solubility of CCDs can be attributed to the presence of abundant hydrophilic groups on their surfaces, which also confirmed the existence of Zn [26]. The chemical composition and functional groups of CCDs were analyzed using X-ray photoelectron spectroscopy (XPS). The XPS full spectrum in Fig. 1F showed that CCDs are mainly composed of C, N, O, and Zn elements. The high-resolution XPS spectrum of C1s can be decomposed into three peaks with binding energies of 288.1 eV, 255.5 eV, and 284.5 eV, respectively. These peaks represented C = O/C-N, C-O/C-N, and C-C/C = C, respectively (Fig. 1G). The N1s band deconvolution peaks at 399.9 eV and 399.0 eV correspond to graphite nitrogen and pyrrole nitrogen, respectively (Fig. 1H) [27]. The peaks of O1s at 532.3 eV and 530.9 eV correspond to C = O and O-H (Fig. 1I) [26]. Fig. 1J showed the high-resolution XPS spectrum of Zn2p, with two peaks at binding energies of 1044.4 eV and 1021.4 eV. These peaks corresponded to the spin orbit dipoles of Zn 2p3/2 and Zn 2p1/2, respectively, indicating that zinc doped CCDs contain zinc in the two positive valence state [28]. The abundant nitrogen in CCDs comes from polyethyleneimine, which can provide the necessary elements for the synthesis of carbon dots. Meanwhile, nitrogen atom doping, as an efficient and convenient method, provides abundant active sites and functional groups on the surface of CCDs, which broadens the application scope of carbon dot nanomaterials. Because the doping of nitrogen plays an important role in improving the fluorescence properties and photosensitizing activity of carbon dots, it may lead to a 20 nm redshift of the maximum fluorescence emission position of the carbon dots and an increase in the emission intensity of the carbon dots, a property that is of great significance for the use of carbon dots as photosensitizers [29]. All these results demonstrated the successful synthesis of Zn-CCDs nanoparticles.
Antibacterial property
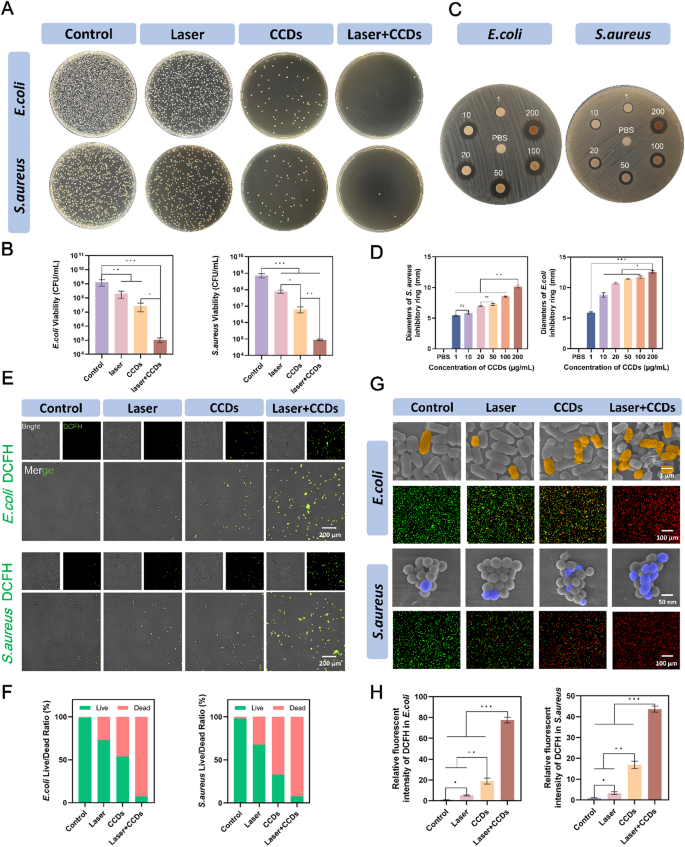
Due to the damaged barrier, exposing the wound to the complex daily environment increases the risk of bacterial infection. S. aureus is ubiquitous on the surface of the skin and in the living environment and is one of the most common infectious agents of the skin [30, 31]. In addition, many studies have shown that E. coli is increasing the incidence of wound infections [32, 33]. Therefore, S. aureus and E. coli were selected as representative strains of Gram-positive and Gram-negative bacteria for the study of the antimicrobial properties of CCDs in PDT of infected wounds. The CCDs composites with an overall positively charged nature were firmly attached to the negatively charged bacterial surfaces by electrostatic interaction. At the same time, a part of the bacteria ingested the nanoscale CCDs into the intracellular space, and PDT effect was produced under laser irradiation to achieve the killing effect. As shown in Fig. 2C, different concentrations of CCDs formed inhibitory rings with varying diameters, indicating that the inhibitory effect of CCDs on bacteria was stronger as the concentration increased (1–200 µg/ml). Digital photographs of S. aureus and E. coli forming colonies on agar plates in different treatment groups are shown in Fig. 2A. The number of colonies in the Laser + CCDs group was significantly less than that of the control group, with a reduction of 3–4 orders of magnitude. It can be seen that laser irradiation or CCDs alone had some inhibitory effect on the growth of both bacteria, but the effect was poor.
Antimicrobial properties. (A) Plate count images of E. coli and S. aureus in each group; (B) Quantitative analysis of the number of E. coli and S. aureus colonies; (C) Ring of inhibition images of E. coli and S. aureus in each group. The different conditions are PBS buffer or CCDs solution with concentrations of 10, 20, 50, 100, 200 µg/mL; (D) Quantitative analysis of diameters of inhibition ring of E. coli and S. aureus with different concentration of CCDs; (E) ROS probe fluorescent staining images of E. coli and S. aureus in each group; (F) Quantitative ratios of live and dead E. coli and S. aureus; (G) SEM images and live/dead fluorescent staining images of E. coli and S. aureus in each group; (H) Quantitative analysis of the intensity of ROS fluorescence of E. coli and S. aureus. (*p < 0.05, **p < 0.01, ***p < 0.001)
CCDs, as a novel photosensitizer, are capable of producing ROS under laser irradiation for photodynamic effects. In order to investigate the specific mechanism of bacterial killing by Laser + CCDs, we used DCFH-DA as a reactive oxygen probe to probe the ROS production in bacteria after different treatments. The presence of ROS in bacteria oxidizes the non-fluorescent DCFH-DA to the strong green fluorescent substance DCF [34]. Fig. 2E showed a weak green fluorescence in E. coli and S. aureus after ingestion of CCDs, and a bright green fluorescence in almost all bacteria after PDT, representing the production of a large amount of ROS after photodynamic therapy. Fig. 2G showed the SEM images of the two bacteria after PDT, with pseudo-colors being used to highlight the regions of interest. It can be seen that the surface of the bacteria in the Control group was smooth and full, with clear and intact boundaries, able to form a complete biofilm structure. In the Laser + CCDs group, it was obvious to see that the bacterial cell membranes were wrinkled, collapsed, with blurred boundaries, and in some cases the contents were in the form of a jet, which is a typical manifestation of the severe damage to the bacteria caused by the high concentration of ROS. The surface of S. aureus was twisted and compressed and deformed, but basically remained intact and spherical. In contrast, the degree of destruction of E. coli was more significant, the cell membrane was strongly contracted and ruptured, and the shell lost its intact morphology. This difference may be due to the fact that the phosphomimic acid cell wall of the outer layer of Gram-positive bacteria restricted the expansion and rupture of the bacterial body to a certain extent. A part of the large amount of ROS generated by photodynamic force acted directly on the cell membrane structure, while the other part attacked the organelles and nucleic acids, causing irreversible damage and thus killing the bacteria. This is the classic type I mechanism in PDT, which played an important role in the whole treatment system [35]. This therapeutic mechanism significantly slowed the development of bacterial drug resistance and prevents the formation of bacterial biofilms. We hypothesize that Zn2+ was released from the composite nanoparticles and disrupted the cell membrane by neutralizing the negative charge of the cell membrane [36]. At the same time, the composition of CUR can also inhibit the adhesion of bacteria to a certain extent, greatly reducing the risk of bacterial infection [37].
In Fig. 2G, live/dead fluorescence staining was performed on the bacteria in different treatment groups to visually distinguish the survival status of bacteria by red and green fluorescence. Compared with the Control group and the Laser group, the rest of the treatment groups had obvious red fluorescence, indicating that the inactivated bacteria accounted for a great proportion. In contrast, there was almost no green fluorescence in the Laser + CCDs treatment group, and this killing showed the same trend in the quantitative analysis of Fig. 2F. Some studies have already reported that PDT has different selectivity for Gram-negative and Gram-positive bacteria due to differences in the surface structure of bacterial cell membranes. In general, photosensitizers are more likely to penetrate the porous cell walls of Gram-positive bacteria to produce ROS to act as bactericidal agents [38, 39].
Exploration of the mechanism of CCDs-mediated PDT also revealed that the ROS produced by this treatment modality inhibits the formation of bacterial biofilm, which improves the permeability of CCDs and enhances the killing effect on deep-seated bacteria [40]. At the same time, this treatment reduces the risk of developing drug resistance by not targeting the characteristic stages of the bacterial metabolic phase and impeding the formation of biofilm——the barrier. The results of biofilm formation inhibition experiments showed (Fig. S2) that the density and structure of the two bacterial biofilms were significantly disrupted after Laser + CCDs treatment and antibiotic Ciprofloxacin treatment, showing almost the same trend, indicating that the effect of CCDs-mediated PDT is almost comparable to that of the standard antibiotics in terms of antimicrobial activity. Therefore, CCDs as photosensitizers can effectively induce ROS burst to inhibit biofilm formation and significantly kill bacteria.
Fig. S3 showed the results of flow cytometry analysis of CCDs mediated PDT on E. coli and S. aureus. It can be seen that almost all (99.1%, 99.5%) of the bacteria in the control group did not undergo apoptosis, which means that most of the bacteria in the group were in a viable state. Both the Laser group (3.34%, 8.17%) and the CCDs group (19.5%, 20.4%) showed varying numbers of stained cells with apoptotic signals, but apoptotic signals were stronger in the CCDs group, which means both of the treatments can both kill certain bacteria, but the killing ability of CCDs is stronger. After the addition of laser irradiation, the survival rate of both bacteria in the Laser + CCDs group decreased dramatically, showing similar results to the antibiotic Ciprofloxacin. Among them, the apoptotic cells of E. coli increased to 32.3% (37.8% in the Ciprofloxacin group) while those of S. aureus increased to 31.4% (36.9% in the Ciprofloxacin group). The results showed that CCDs-mediated PDT had excellent antibacterial effects, even similar to those of standard antibiotics, and was effective in inducing apoptosis and inhibiting further propagation of bacteria. CCDs adhered to the bacterial organisms and entered into the intracellular compartment, and then ROS generated by the PDT damaged the internal biomolecules of bacteria and eventually led to bacterial death, which is in line with the conclusions drawn from the previous studies [41].
Promote cell migration and vascularization
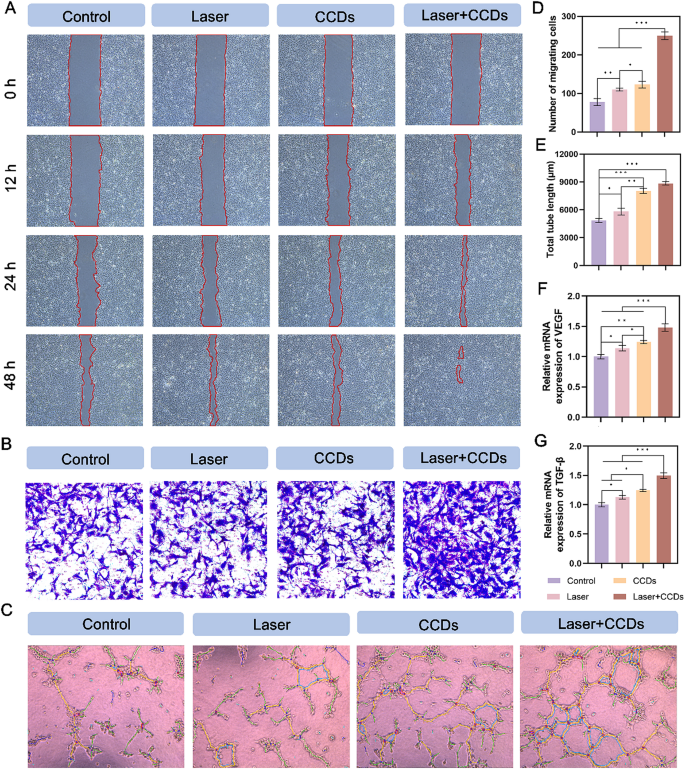
Damaged tissues begin to proliferate and repair after the inflammatory phase, and blood vessels are important channels for transporting nutrients and growth factors [42]. Classical scratch and transwell migration assays were chosen to examine the angiogenic potential of HUVEC and L929 cells after PDT, and a matrigel-based tube formation assay for HUVEC was designed to further investigate.
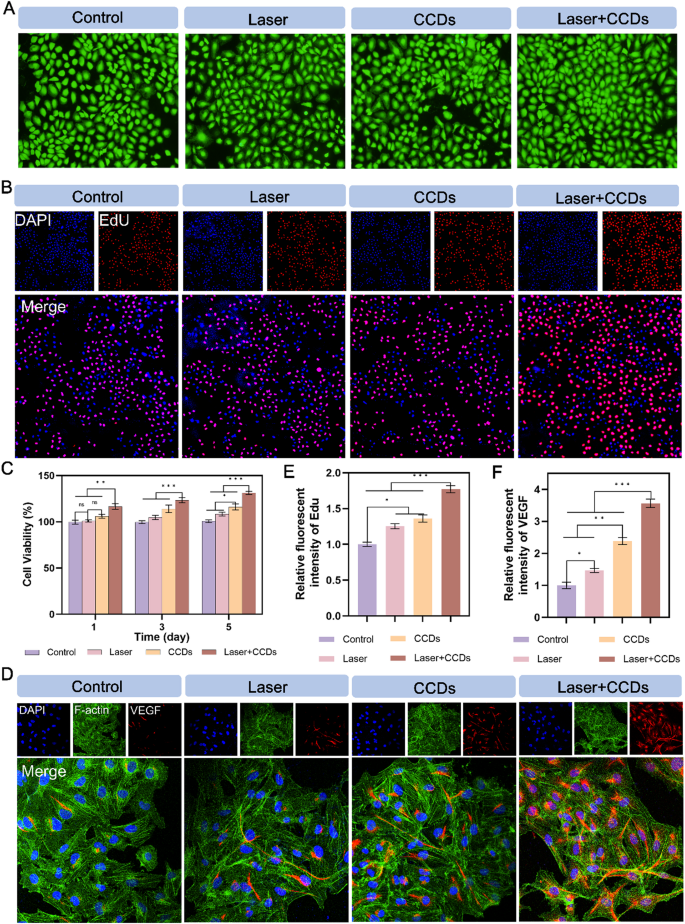
The cytotoxicity of CCDs was first explored by standard CCK-8 assay. Fig. S4 showed that CCDs at different concentrations did not exhibit significant toxicity after 1, 3 and 5 days of co-culture with HUVEC. Interestingly, CCDs at a concentration of 200 µg/ml were able to significantly promote the proliferation of endothelial cells to some extent. This concentration was chosen as the standard concentration for subsequent assays. Fig. 3C and Fig. S5 showed that the Laser + CCDs treatment group promoted the proliferation of HUVEC and L929 cells, respectively. The CCDs treatment group also slightly raised the viability of both cells. The remaining treatment groups showed no significant difference. Based on the results of live/dead cell staining of HUVEC cultured with CCDs for 24 h, almost no dead cells (red fluorescence) were observed in each treatment group, as shown in Fig. 3A. EdU staining of HUVEC showed similar results to those of CCK-8. EdU is a thymine deoxyribonucleoside analog that is capable of replacing the thymine deoxy nucleus doped into de novo and synthesized DNA during DNA synthesis. Therefore, the amount of newly synthesized DNA was examined by the EdU-related kit to reflect the proliferation status of the cells. The results showed (Fig. 3B) that the Laser + CCDs group exhibited bright red fluorescence, and the rest of the treatment groups had weaker fluorescence intensity (Fig. 3E), indicating that CCDs in the presence of laser irradiation could indeed promote HUVEC propagation and facilitate wound recovery.
Promotion of HUVEC proliferation and angiogenic protein expression. (A) Live/dead staining images of HUVEC; (B) Fluorescence images of HUVEC EdU staining in each group; (C) Cell proliferation in CCK8 assay at 1, 3 and 5 days; (D) Immunofluorescence staining images of VEGF protein in each group; (E) Quantitative analysis of fluorescence intensity of EdU staining in each group; (F) Quantitative analysis of immunofluorescence intensity of VEGF protein in each group. (*p < 0.05, **p < 0.01, ***p < 0.001)
Scratch healing by endothelial cells is central to the process of tissue re-formation during wound healing. As shown in Fig. 4A and Fig. S6A, both HUVEC and L929 cells in the Laser + CCDs group exhibited optimal healing after treatment. Notably, the CCDs group also showed some promotion in the scratch assay for both cells. The data in Fig. S5 and Fig. S6D quantified the healing rate of scratches, showing the same trend. After 24 h of incubation, the migration rates of HUVEC and L929 cells were significantly higher in the Laser + CCDs group than in the other treatment groups (Fig. 4B and S6B). Endothelial cells are components of blood vessels and play a crucial role in angiogenesis. The matrix gel tube formation assay performed to assess the angiogenic capacity showed (Fig. 4C) that Laser + CCDs-treated HUVEC showed a significant increase in tube length and number of junctions after 6 h compared with the Control group (Fig. 4E and S8), which may be attributed to the release of Zn2+ as well as the generation of controlled ROS. Overall, CCDs have the ability to promote cell migration under laser irradiation, which is beneficial for accelerating the wound healing process.
Promotion of HUVEC migration and angiogenic property. (A) Representative images of HUVEC scratching assay, the red underlined portion represents the scratched area; (B) Representative images of HUVEC transwell migration assay in each group; (C) Images of HUVEC tube formation assay; (D) Quantitative analysis of the number of migrating cells in each group; (E) Quantitative analysis of the total tube length formation in each group; (F) Quantitative analysis of relative mRNA expression of VEGF; (G) Quantitative analysis of relative mRNA expression of TGF-β. (*p < 0.05, **p < 0.01, ***p < 0.001)
As a well-known angiogenesis related factor, vascular endothelial growth factor (VEGF) induces proliferation, migration, and angiogenesis of epidermal and endothelial cells. During angiogenesis, VEGF is essential for the recruitment, maintenance, proliferation, migration and differentiation of endothelial cells [43, 44]. Therefore, we expressed the expression of VEGF protein in cells of different treatment groups by fluorescence staining (Fig. 3D and S6C). The results showed that HUVEC and L929 cells exhibited bright red fluorescence in the cytoplasm after PDT, and CCDs-treated group also had strong red fluorescence, while the ones in the Control group showed almost no expression. The quantitative analysis of fluorescence intensity in Fig. 3F and Fig. S6F is consistent with the above. The relative gene expression levels of VEGF and TGF-β in the two types of cells (Fig. 4F and G and S9, S10) were closer in the CCDs and Laser + CCDs groups, and significantly higher than those in the Control and Laser groups. Zinc, as an essential trace element, plays an important biological function in the maintenance of the venous vascular network and the development of hematopoiesis [45]. Our study confirmed that CCDs stimulate angiogenesis by slowly releasing Zn2+, which is consistent with previous reports [46]. And the aforementioned toxicity test also showed that Zn2+ in the composite nanoparticles also did not affect the normal cell viability. The above results indicated that CCDs exhibit complex and active regulation of angiogenesis after laser irradiation.
The potential mechanism of accelerated infected wound healing
Wound healing is a complex process involving interactions between different cell types, growth hormones, cytokines, antioxidants, and a steady supply of metal ions (e.g., calcium, zinc, and magnesium). After skin damage, a number of cellular systems and signaling pathways are activated in the wound to protect the body [47]. In order to elucidate the possible regulatory mechanisms of Zn2+-doped curcumin carbon dots to promote infected wound healing, we performed transcriptome analysis on cells from two different treatment groups (Control and Laser + CCDs groups).
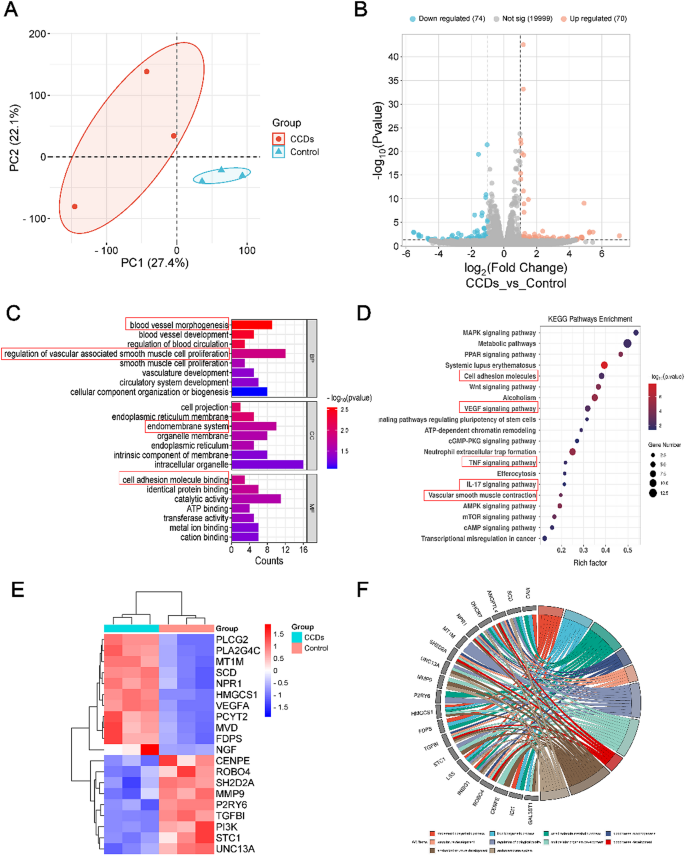
Principal Component Analysis (PCA) results showed that samples from each group were clustered independently, verifying that the two treatment groups did produce differences (Fig. 5A). Volcano plots showing up- and down-regulated genes generated after different treatments in the Control and Laser + CCDs groups exhibited significant differential gene expression between the different groups (Fig. 5B). To further analyze these differential gene expressions, we performed Gene Ontology (GO) enrichment analysis. GO typically characterizes genes at three levels: cellular component (CC), biological process (BP), and molecular function (MF). Fig. 5C showed the top enriched items in each category, which mainly include down-regulated expression of immune response, inflammatory response aspects and up-regulated vascular morphology and proliferation of vascular smooth muscle, endothelial phylogeny and cell adhesion.
Gene expression profiles and regulatory mechanisms in promoting infectious wound healing. (A) PCA analysis of samples; (B) Volcano plot with up- and down-regulated genes; (C) Representative top 22 differentially expressed terms analyzed by the Gene Ontology (GO) enrichment method; (D) Representative top 20 up- or down-regulated pathways analyzed by KEGG pathway method; (E) The Heatmap analysis and (F) circus of differentially expressed genes involved in multiple pathways
Meanwhile, Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis was applied to analyze the potential signaling pathways. Fig. 5D showed in detail the pathways with high relevance and their names, and the up-regulated signaling pathways include VEGF signaling pathway, cell adhesion molecule signaling pathway and mitogen-activated protein kinase (MAPK) signaling pathway.
It is well known that the VEGF signaling pathway is closely related to collagen deposition and angiogenesis. And the MAPK signaling pathway promotes keratinocyte proliferation and migration, and plays an important role in transmitting extracellular stimulatory signals to cells and mediating cellular biological responses (e.g., cell growth, migration, proliferation, differentiation, and apoptosis). On the other hand, CCDs photodynamic therapy also down-regulated some of the pathways, including the IL-17 signaling pathway, and the tumor necrosis factor (TNF) signaling pathway, which are associated with the inflammatory response and regulation of tissue destruction. The heatmap in Fig. 5E showed the names of the genes with specific changes for major differences in the above pathways. Specific names and interconnections regarding the genes screened for greater differential expression by GO enrichment analysis are displayed in Fig. 5F. These results suggested that the VEGF signaling pathway may be activated during PDT with CCDs to promote cellular angiogenesis, thereby accelerating wound healing.
MAPK is very important in transmitting signals of extracellular stimuli to the cells and mediating cellular biological responses (e.g., cell growth, migration, proliferation, differentiation and apoptosis). Mammalian MAPKs can be categorized into four subfamilies: ERK1/2, p38, JNKs and ERK5 [48]. Multiple differential genes of the ERK pathway were enriched in the MAPK signaling pathway. VEGF is the most important angiogenic stimulator and plays important roles in angiogenesis and neointima formation, including causing cell proliferation, inhibiting apoptosis, increasing vascular permeability, and vasodilation. Genes upregulated in the VEGF/VEGFR2 pathway include VEGFA, PLCG2, and PLA2G4C. Among them, PLA2G4C is also involved in the ERK pathway.
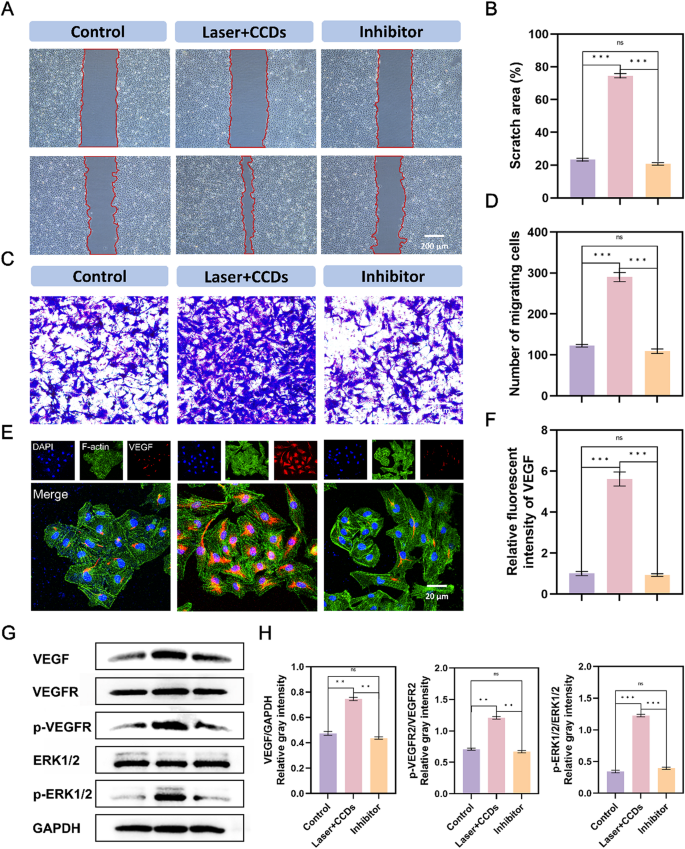
To investigate whether the MAPK and VEGF signaling pathways were potential mechanisms and further validate the above hypothesis to promote infectious wound healing, we validated them in terms of genes and proteins as well as phenotypes. VEGFR2 inhibitor (SU19498) was used to test the reliability of the sequencing results. The scratch test results after 12 h in Fig. 6A showed that the scratch area of the Control group and the Inhibitor group has not changed much compared to 0 h, with only a trace amount of healing. The Laser + CDs group showed a significant promoting effect on healing. The migration assay in Fig. 6C also showed the same trend, with only the Laser + CCDs group showing a large number of cells migrating to the lower chamber. This proves that VEGFR2 inhibitor hindered the signaling process on this pathway, thereby inhibiting the growth and migration of HUVEC cells. The above effects were also demonstrated by VEGF immunofluorescence and immunoblotting (Fig. 6E and G), confirming the importance of VEGF in endothelial cell growth and various physiological activities. The VEGF/VEFGR2 pathway is closely related to the MEK1/2/ERK1/2 signaling pathway, and one of the downstream pathways of the VEGF signaling pathway is to mediate cell proliferation through the ERK pathway [49]. By WB detection of VEGF, VRGFR2, phosphorylated VRGFR2, phosphorylated ERK1/2, and ERK1/2, we found that the protein expression levels of the Control group and pathway inhibitor group were almost the same, whereas the expression of each index was significantly increased in the PDT group with CCDs. It is particularly noteworthy that the application of VEGFR2 inhibitor (SU19498) can effectively inhibit the phosphorylation of VEGFR2, resulting in a significant decrease in the expression levels of downstream VEGF proteins p-VEGFR2/VEGFR2 and p-ERK1/2/ERK1/2 in the Inhibitor group. In summary, the above results indicated that CCDs promote endothelial cell growth and wound healing through the VEGF/VEGFR2/ERK1/2 pathway.
Verification of VEGF signaling pathway mechanism in HUVEC. (A) Representative images of scratching assay, the red underlined portion represents the scratched area; (B) Quantitative analysis of scratch area closure in each group; (C) Representative images of migration assay in each group; (D) Quantitative analysis of the number of migrating cells in each group; (E) Immunofluorescence staining images of VEGF protein in each group; (F) Quantitative analysis of immunofluorescence intensity of VEGF protein in each group;(G) Expression of VEGF, VEGFR, ERK1/2, phospho-VEGFR, -ERK1/2 and GAPDH, as well as the gray intensity analysis in HUVEC; (H) Quantitative analysis of (G). (*p < 0.05, **p < 0.01, ***p < 0.001)
The results suggested that CCDs photodynamic therapy exerts its role in promoting vascular endothelial cell growth by modulating VEGF/VEGFR2 and its downstream MEK1/2/ERK1/2 signaling axis. Thus, wound healing cannot be achieved without precise regulation including hemostasis, inflammation, proliferation and remodeling sequences.
Evaluation of in vivo infected wound healing
Based on the efficacy of CCDs with PDT in killing bacteria and promoting the proliferation and repair of endothelial cells obtained in vitro, we further used infected wound rats to study their repair effect in vivo.
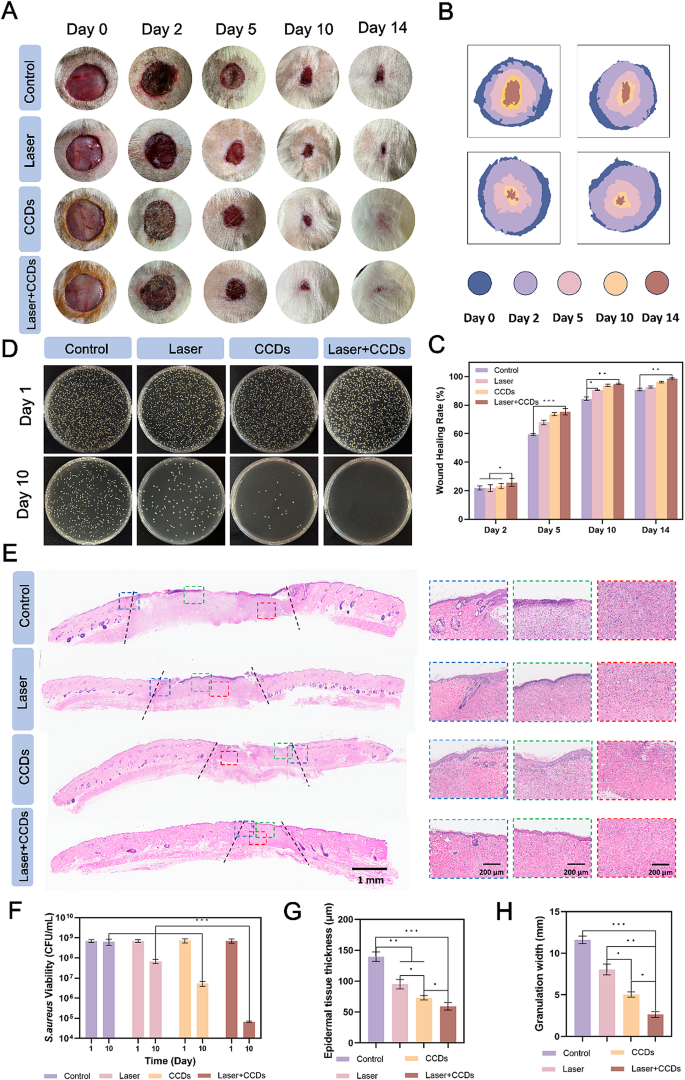
First, a whole-layer rat skin defect model with a diameter of 2 cm was created, and S. aureus bacterial suspension was applied to the wound surface to establish an infection model. Saline and CCDs were injected into the infected wounds for treatment (named Control group, Laser group, CCDs group, and Laser + CCDs group, respectively), and the parameters of the laser used in the treatment were 660 nm, 10 min, and 500 mW/cm2. Digital photographs of the wound area at different time points and overlapping images of the simulated healing are shown clearly in Fig. 7A and B. After 24 h, the wound the wound became visibly infected. The results showed that at the end of the first treatment (day 2), the surface of the Control and Laser groups was ulcerated and oozing, bleeding was apparent, and no obvious scab formation was seen, while the CCDs and Laser + CCDs groups showed obvious signs of healing, with the bleeding stopping and the formation of thicker healing scabs. After 14 days, the wounds of the CCDs and Laser + CCDs groups were almost healed but accompanied by varying degrees of scar formation. In contrast, wounds in the Control and Laser groups remained open, and the newly formed tissue was significantly thinner and redder. The percentage of wounds healed in each group of rats is quantified in Fig. 7C. Significant differences were observed between groups after 2 days, with the Control group having the slowest healing rate values at all time points. 92.65%, 96.05%, and 98.7% of wounds were healed at the last time point in the Laser group, the CCDs group, and the Laser + CCDs group, respectively. To directly characterize the infection, tissues from the wound area were homogenized and incubated on agar plates. Fig. 4D and F showed the colony diagrams and quantitative results of localized bacteria in all wounds after day 1 and day 10, respectively. The results showed that a large number of colonies with surface bacterial colonization and growth were observed in all treatment groups at day 1. Whereas, on day 10, the number of colonies in the Laser + CCDs group was significantly reduced, and quantification showed that S. aureus was reduced by almost 4 orders of magnitude. The above results indicated that PDT with CCDs has the potential to control wound infection and assist healing.
Infected wounds healing in vivo. (A) Representative digital photographs of each group of wounds at day 0, 2, 5, 10, and 14; (B) Schematic representation of overlapping wound areas at representative time points; (C) Quantification of the closed wound area percentage; (D) Plate count images of S. aureus of wounds in each group at day 1 and 10; (E) Representative images of the H&E staining in each group, showing skin tissue, the overall structure of the neoplastic epithelium at the wound edge (in the blue dashed box), the epithelium in the center of the wound (in the red dashed box), and the subepithelial layer (in the green dashed box); (F) Quantitative analysis of the number of S. aureus colonies in each group; (G) Quantitative analysis of the newborn epithelial tissue thickness and (H) the granulation tissue width in each group. (*p < 0.05, **p < 0.01, ***p < 0.001)
In addition, to further explore the complex biological processes including inflammation, proliferation, and remodeling during the healing of infected wounds treated with CCDs.
in PDT, we evaluated the histological changes after 14 days. At day 14 post-treatment, hematoxylin-eosin (H&E) staining of the wound and surrounding area showed histologically relevant wound healing, such as epithelial re-formation and granulation tissue, as shown in Fig. 7E. The results of the H&E staining of the wound and surrounding area showed that the wound healing process was not as simple as that of the Control group. The granulation tissue width (distance between the black dotted lines) was significantly reduced in the CCDs group and narrowest in the Laser + CCDs group compared to the Control and Laser groups, with quantitative results showing the same trend (Fig. 7H). The blue dashed box in Fig. 7E showed the normal epithelium versus the damaged epithelium, and it can be seen that the photodynamically treated tissues appeared as smooth and flat epithelium with neoplastic hair follicles, which is closer to the state of normal skin. In contrast, the other treatment groups had disorganized cells in the basal layer, disorganized collagen, and clear demarcation from the normal epithelium. The red dashed box illustrated the reduction of inflammatory cell infiltration and the appearance of more fibroblast migration in the epithelium in the Laser + CCDs group after photodynamic treatment. The green dashed box showed that the control group had edema, discontinuity and dense inflammatory cell bands in the epithelium. The Laser + CCDs group had a thinner epithelium with no visible inflammatory cells and more mature tissue remodeling. Quantitative analysis of epithelial tissue thickness was shown in Fig. 7G. Thicker epithelial tissue thickness was observed in the Control group (138 ± 12 μm) and Laser group (94 ± 7 μm).
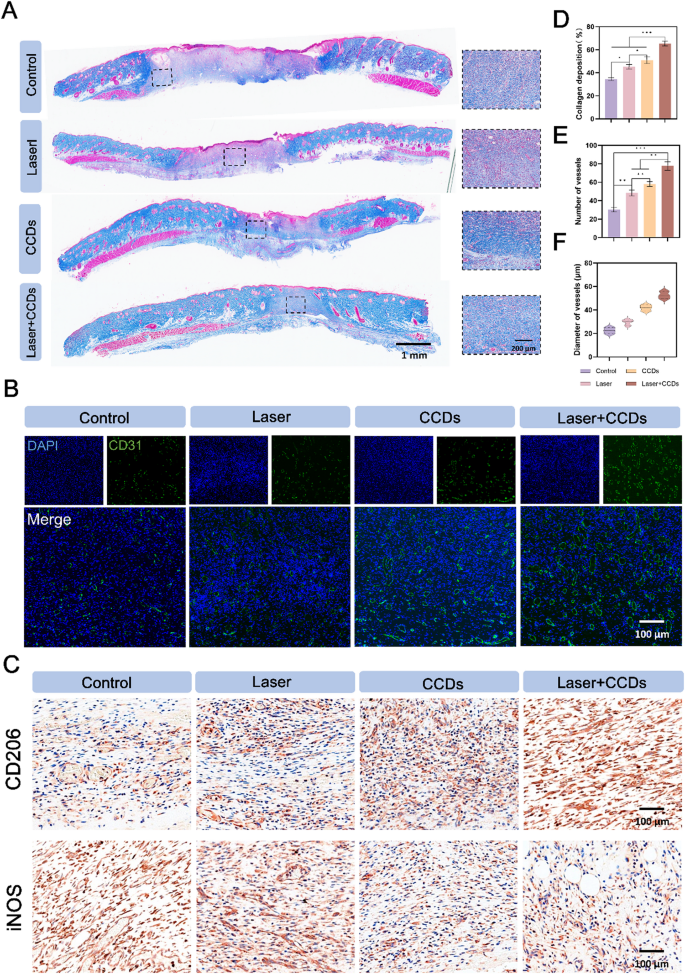
Collagen deposition is a key determinant of skin strength and maturity [50]. Masson staining in Fig. 8A gave a more specific picture of the amount of collagen in the newborn skin tissue and the arrangement of its fibers. The collagen fibers in the CCDs group and the Laser + CCDs treatment group were more dense, well-arranged, and the tissue was more mature. Quantitative analysis of collagen deposition in Fig. 8D showed the same results. The major collagens in the skin are collagen types I and III, which make up about 95% of the skin’s collagen composition. These two types of collagens play an important role in maintaining the elasticity, integrity and pliability of the skin. Not only that, but these two most important types of collagens are also under dynamic change during the wound healing process in addition to the increase in the overall amount of collagen [51]. Therefore, Sirius red staining was utilized to differentially stain mainly type I (red/yellow) and type III (green) collagens based on the different characteristics of collagen polymerization winding and helical arrangement. The results showed (Fig. S11) that at day 7, a lower proportion of type I and type III collagen was observed in the Laser + CCDs group, with an overall green-dominated fluorescent signal, which was due to the fact that type III collagen was more predominant in the early wound healing stage. In the process of wound remodeling and tissue maturation, type III collagen was gradually replaced by mature type I. The Laser + CCDs group showed a similar proportion of type I and type III collagen as normal skin on day 14, and the overall fluorescence signal was reddish-yellow, which indicated that the wound healing after PDT tended to be normalized during reconstruction and remodeling, and there was no delayed and disordered collagen deposition.
(A) Representative images of Masson staining; (B) Immunofluorescence staining images of CD31 expression in each group; (C) Representative immunohistochemical staining images of CD206 and iNOS expression in each group; (D) Quantitative analysis of collagen deposition in each group; (E) Quantitative analysis of blood vessel number and (F) diameter in each group. (*p < 0.05, **p < 0.01, ***p < 0.001)
The blood vessels in the new tissue can deliver essential nutrients, growth factors and oxygen to the wound site, and CD31 is a typical marker for vascular endothelial cells [52]. As shown in Fig. 8B, the immunofluorescence images showed that the Control and Laser groups showed few green fluorescent signals, while the CCDs and Laser + CCDs treatment groups showed more signals and more complete green fluorescent rings. Therefore, we analyzed the number and diameter of blood vessels (Fig. 8E and F) and found that can CCDs group and Laser + CCDs treatment group promoted the formation of vascular system. Zn2+ in the composite nanoparticles induced proliferation, migration and angiogenesis of epidermal and endothelial cells [53]. The inflammatory response period is a stage in normal wound healing, and we explored the inflammatory changes during wound healing by evaluating two typical inflammation-related factors. In Fig. 8C, the anti-inflammatory factor CD206 was shown to be barely expressed in the control group, while the expression showed an increasing trend in the Laser, CCDs and Laser + CCDs treatment groups, and the pro-inflammatory factor iNOS showed a completely opposite expression in the four treatment groups. The indication suggested that PDT effectively increased the anti-inflammatory level in vivo and significantly reduced inflammation. The above results suggested that CCDs promote healing of infected wounds by accelerating the blood supply for neovascularization as well as decreasing the level of inflammation through photodynamic therapy. At the end of the animal experiments, H&E staining of major organs was performed (Fig. S14). There were no differences between all treatment groups, suggesting that CCDs were non-toxic and well biologically safe in vivo and can significantly promote infected wound healing in a safe manner.